您經常受尿頻、尿急、夜尿困擾嗎?
您有尿頻、夜尿、排尿困難等問題嗎?我們統稱這些問題為「下泌尿道症狀」 (LUTS)。根據香港中文大學一個電話訪問調查,受訪者中有七成多的40歲以上男女都曾患有「下泌尿道症狀」。1 不少人以為年紀大,這些問題無可避免,或因感到尷尬而遲遲未求醫。事實上,這些症狀不但影響患者日常生活,長遠更有機會造成心理壓力,甚至拒絕社交活動,2影響深遠。長者頻頻夜尿更可能增加跌傷和骨折的風險。3在香港,高達17%的50歲以上患者會於髖骨骨折一年內死亡。4
您長期受「下泌尿道症狀」困擾嗎?不用擔心,現時有不少藥物,能有效舒緩病情。因此及早了解和治療相當重要!

甚麼是「下泌尿道症狀」(LUTS)?
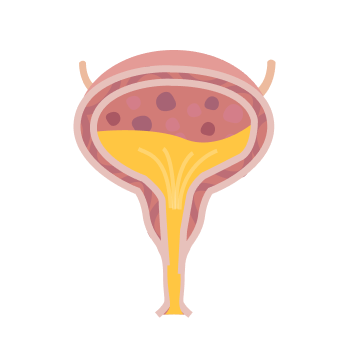
「下泌尿道症狀」 (LUTS) 指下泌尿道(包括膀胱、前列腺及尿道)問題的各類症狀,其中包括男女均有機會患上的「膀胱過度活躍症」(Overactive Bladder,OAB)和只有男性有機會患上的「良性前列腺增生」(Benign Prostatic Hyperplasia,BPH)。5
「膀胱過度活躍症」(OAB) :
膀胱儲存尿液功能出現問題。6膀胱未達到正常排尿容量時,便不正常地突然收縮,增加膀胱內的壓力,造成突發性尿急、尿頻。7患者或需立刻如廁,嚴重時更有機會尿失禁(漏尿)。8部份患者亦會出現尿頻、夜尿等症狀。6
「良性前列腺增生」(BPH) :9
指男性前列腺有增生的現象,以致排尿功能出現問題,如排尿時比較費力,尿流細弱或斷續。患者大多需等候一段時間,才能開始排尿,而且尿液快要排盡前,尿流會變成尿滴。年紀越大的男性,患「良性前列腺增生」症的機會就越高。
很多男性出現尿頻時,以為自己患上「良性前列腺增生」。事實上,他們有可能是患上了「膀胱過度活躍症」,甚至可能同時患上兩種泌尿系統疾病。10 根據一項歐美的研究,約每三個患有「下泌尿道症狀」的40歳或以上男性中,就有一個同時有儲存和排尿問題。10
近年已有不少新藥物,如Beta-3腎上腺素受體激動劑(β3-agonists)可放鬆膀胱肌肉,增加膀胱儲尿能力,改善尿頻、尿急、夜尿、尿失禁等症狀。11, 12, 13 相比過往採用的抗乙醯膽鹼劑,β3腎上腺素受體激動劑出現口乾等副作用的機會較低 。14此外,近年亦有研究顯示β3腎上腺素受體激動劑對於長者沒有出現認知能力的副作用。15
而對α-1a和α-1d受體選擇性比較高的α1-受體阻滯劑 (α1-Blocker) 除了可同時放鬆前列腺和膀胱頸的平滑肌,改善排尿因難等症狀外16,心血管及頭暈方面的副作用亦較低。17, 18

至少有1種儲存、排尿及排尿後症狀10
患有「膀胱過度活躍症」19

就有2個 有中度至重度
「良性前列腺增生」20

我有「下泌尿道症狀」嗎?
此測試由「膀胱過度活躍症」症狀問卷(OABSS)21和國際前列腺症狀評分表(IPSS)22組成,協助您作出初步評估。只需回答數條簡單選擇題(男士回答12條,女士回答5條),就可了解自己的情況。






- [1]Yee, C. H., Chan, C. K., Teoh, J. Y., Chiu, P. K., Wong, J. H., Chan, E. S., ... & Ng, C. F. (2019). Survey on prevalence of lower urinary tract symptoms in an Asian population.Hong Kong Med J,25(1), 13-20.
- [2]Milsom, I., Kaplan, S. A., Coyne, K. S., Sexton, C. C., & Kopp, Z. S. (2012). Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression,and treatment seeking in the United States: results from EpiLUTS.Urology,80(1), 90-96.
- [3]Hwang, T. Y., Kim, S. K., Kim, K. H., & Kim, J. Y. (2019). Association between lower urinary tract symptoms and falls in adults males: based on the Korean Community Health Survey.Asia Pacific Journal of Public Health,31(7), 643-651.
- [4]Leung, K. S., Yuen, W. F., Ngai, W. K., Lam, C. Y., Lau, T. W., Lee, K. B., ... & Cheung, W. H. (2017). How well are we managing fragility hip fractures? A narrative report on the review with the attempt to setup a Fragility Fracture Registry in Hong Kong.Hong Kong Med J,23(3), 264-271.
- [5]Chapple C. (2011). Chapple C. (2011). Systematic review of therapy for men with overactive bladder.Canadian Urological Association journal = Journal de l'Association des urologues du Canada,5(5 Suppl 2),S143–S145. https://doi.org/10.5489/cuaj.11186
- [6]Irwin, D. E., Milsom, I., Hunskaar, S., Reilly, K., Kopp, Z., Herschorn, S., ... & Abrams, P. (2006). Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study.European urology,50(6), 1306-1315.
- [7]Abrams, P., Blaivas, J. G., Stanton, S. L., & Andersen, J. T. (1988). Standardisation of terminology of lower urinary tract function.Neurourology and Urodynamics,7(5), 403-427.
- [8]Keane, D. P., & O'Sullivan, S. (2000). Urinary incontinence: anatomy, physiology and pathophysiology.Best Practice & Research Clinical Obstetrics & Gynaecology,14(2), 207-226.
- [9]Parsons, J. K. (2010). Benign prostatic hyperplasia and male lower urinary tract symptoms: epidemiology and risk factors.Current bladder dysfunction reports,5(4), 212-218
- [10]Sexton, C. C., Coyne, K. S., Kopp, Z. S., Irwin, D. E., Milsom, I., Aiyer, L. P., ... & Wein, A. J. (2009). The overlap of storage, voiding and postmicturition symptoms and implications for treatment seeking in the USA, UK and Sweden: EpiLUTS.BJU international,103, 12-23
- [11]Fest, J., Pfalzgraf, D., Weiss, C., & Hetjens, S. (2017). Evaluating the efficacy and tolerabilitya β3-adrenoceptor agonist, for the treatment of overactive bladder: systematic review and network meta-analysis.Journal of Clinical Urology,10(6), 557-567
- [12]Kuei, C. H., Peng, C. H., & Liao, C. H. (2015). Perspectives in the treatment of overactive bladder syndrome: a new beta-3 adrenoceptor agonist.Urological Science,26(1), 17-23.
- [13]Chapple, C. R., Dvorak, V., Radziszewski, P., Van Kerrebroeck, P., Wyndaele, J. J., Bosman, B., ... & Yamaguchi, O. (2013). A phase II dose-ranging study in patients with overactive bladder.International urogynecology journal,24(9), 1447-1458.
- [14]Kelleher, C., Hakimi, Z., Zur, R., Siddiqui, E., Maman, K., Aballéa, S., ... & Chapple, C. (2018). Efficacy and tolerability compared with antimuscarinic monotherapy or combination therapies for overactive bladder: a systematic review and network meta-analysis.European urology,74(3), 324-333
- [15]Griebling, T. L., Campbell, N. L., Mangel, J., Staskin, D., Herschorn, S., Elsouda, D., & Schermer, C. R. (2020). Effect on cognitive function in elderly patients with overactive bladder: MoCA results from a phase 4 randomized, placebo-controlled study (PILLAR).BMC geriatrics,20(1), 1-10.
- [16]Wilde, M. I., & McTavish, D. (2000). A review of its pharmacological properties and therapeutic potential in the management of distal ureteral stones.Urology,56, 579
- [17]Neill, M. G., Shahani, R., & Zlotta, A. R. (2008). The treatment of benign prostatic hypertrophy.Therapeutics and clinical risk management,4(1), 11.
- [18]Chapple, C. R. (2005). The evolution of the treatment of lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH).European Urology Supplements,4(7), 20-22.
- [19]Chan, C., Yiu, M., & Hou, S. (2010, August). Categorization of the overactive bladder and the related behaviour of seeking medical therapy in the general population—Hong Kong study. InAbstract presented at: Joint Annual Meeting of the International Continence Society (ICS) andInternational Urogynaecological Association(pp. 23-27).
- [20]Yee, C. H., Li, J. K., Lam, H. C., Chan, E. S., Hou, S. S. M., & Ng, C. F. (2014). The prevalence of lower urinary tract symptoms in a Chinese population, and the correlation with uroflowmetry and disease perception. International urology and nephrology, 46(4), 703-710.
- [21]Yiu, M. K., Li, C. M., Hou, S. M., Wong, C. W., Tam, S., & Chu, S. K. (2013). Reliability and validity of the overactive bladder symptom score in Hong Kong Chinese.Hong Kong Med J,19(6), 504-10
- [22]國際前列腺徵狀評分(IPSS). 香港泌尿外科學會. 2018. (Accessed January 12, 2021, at http://www.hkua.org/IPSS/)